Anatomy of the Nose: Structure, Function, and Breathing & Smell, A Clear and Easy Guide
Anatomy of the Nose: Your nose is remarkably more complex than most people realize. However, what looks like a simple projection in the center of your face is actually an intricate three-dimensional structure involving multiple bones, several cartilages, elaborate blood supply, sophisticated neural innervation, and connections to hollow spaces (sinuses) throughout your facial skeleton.
Understanding the anatomy of the nose matters for several reasons. For instance, if you’re considering rhinoplasty, comprehending what surgeons are actually working with helps you make informed decisions and set realistic expectations. Additionally, if you have breathing problems, knowing nasal anatomy clarifies what might be causing them. Furthermore, if you’re simply curious about how your body works, the nose offers a fascinating example of form following function—where aesthetic appearance and physiological purpose are inseparably intertwined.
Let’s explore the anatomy of the nose systematically—from external structures you can see and touch to internal spaces you can’t, from the rigid framework of bones to the flexible architecture of cartilage, and from the vascular networks that bring blood flow to the nerve endings that give you your sense of smell.
External Nasal Anatomy: The Structures You See
The external nose is what you see when you look in the mirror—the projection from your face that gives you your profile and frontal appearance.
The Nasal Regions
The external nose divides into several defined regions:
The nasal root (or radix) is where your nose begins, sitting between your eyebrows at the level of your eyes. Specifically, this is the highest point of the nose, where the nasal bones attach to the frontal bone of your skull.
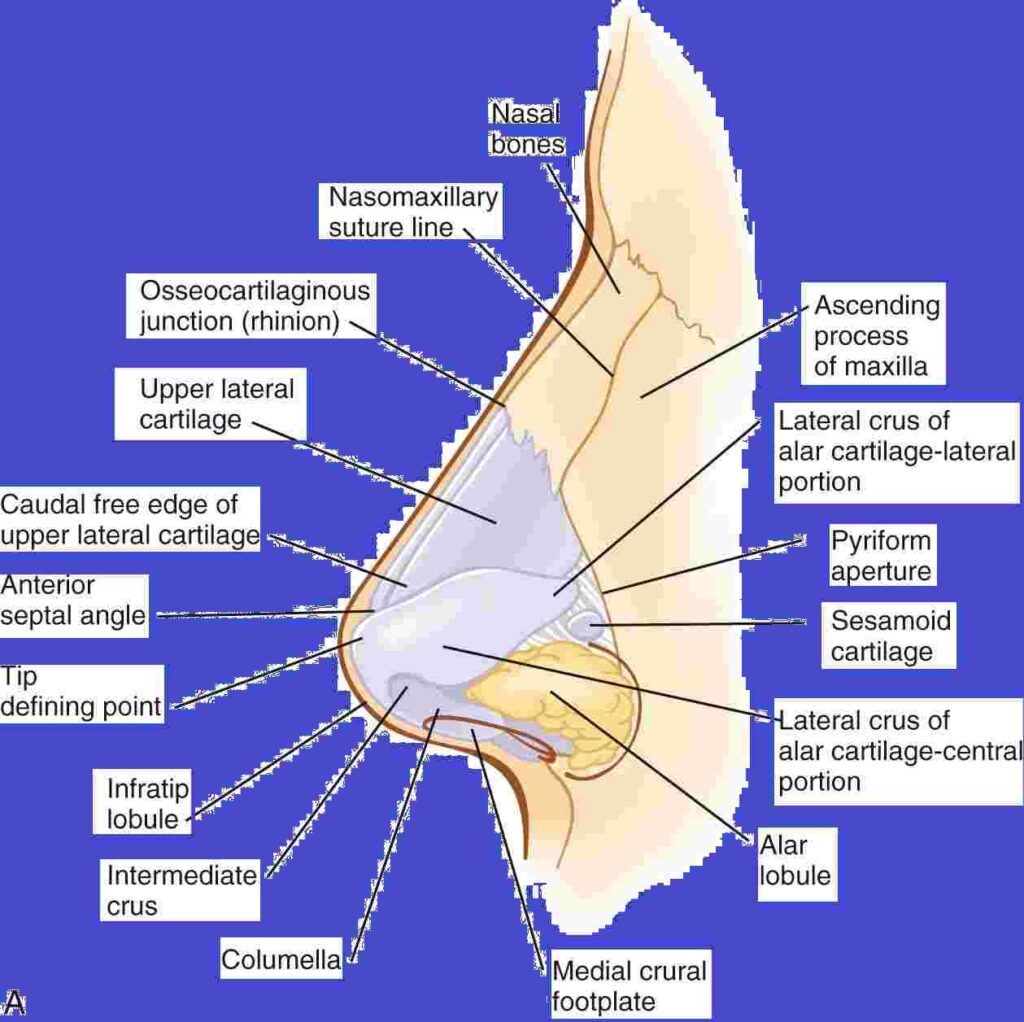
The nasal bridge (or dorsum) extends from the root down toward the tip. Notably, the upper third is bony—formed by the paired nasal bones. In contrast, the middle third is cartilaginous—formed by the upper lateral cartilages and the dorsal septum. Therefore, this is the profile line that people often want to modify with rhinoplasty, whether removing a hump or building up a low bridge.
The nasal tip is the most projected, anterior point of the nose. Specifically, it’s formed entirely by cartilage—specifically, the lower lateral cartilages (also called alar cartilages). Moreover, the tip is also the most technically challenging area for rhinoplasty surgeons to shape predictably.
The columella is the tissue column separating your two nostrils at the base of your nose. In particular, it’s supported by the medial crura (inner portions) of the lower lateral cartilages and the caudal (bottom) edge of the septal cartilage.
The nostrils (or nares) are the external openings of your nasal passages. Consequently, the shape and size of your nostrils are determined by the alar cartilages, surrounding soft tissue, and the width of your nasal base.
The nasal alae are the outer walls of the nostrils—the portions that flare outward when you breathe deeply. Specifically, these are formed by the lateral portions of the lower lateral cartilages plus fibrofatty tissue.
Anatomy of the Nose: The Skin Envelope
The skin on your nose isn’t the same thickness everywhere. In fact, it’s thinner over the bridge and upper part, while the skin around the tip and nostrils is thicker and contains more oil (sebaceous) glands.
This variation matters surgically because thick skin shows less definition of underlying structures—it can “mask” refined surgical work. Conversely, thin skin shows everything, including small irregularities.
The skin is also highly vascular, meaning it has excellent blood supply. As a result, this is why noses heal well after surgery or injury, but it’s also why they bleed profusely when injured.
The Bony Framework: Rigid Structure
The skeleton of the nose combines bone in the upper portion with cartilage in the lower portions.
Anatomy of the Nose: The Nasal Bones
The paired nasal bones form the bony bridge of your nose—roughly the upper third of the external nose. These are thin, rectangular bones that meet in the midline and attach superiorly to the frontal bone (forehead), laterally to the maxillary bones (upper jaw/cheek bones), and inferiorly to the cartilaginous portion of the nose.
The nasal bones are among the most frequently fractured bones in the human body, simply because the nose projects outward and is vulnerable to impact. However, their thinness means they fracture relatively easily, but it also means they heal reasonably well.
In rhinoplasty, surgeons often need to modify the nasal bones through several techniques:
- Rasping or filing to smooth irregularities
- Osteotomies (controlled fractures) to narrow a wide bridge or to close an “open roof” after hump removal
- Additionally, augmentation with grafts if the bridge is too low
The Maxillary Spine and Piriform Aperture
While not part of the nose per se, the anterior nasal spine (a projection of the maxilla at the base of the nose) and the piriform aperture (the pear-shaped bony opening) provide important anatomical landmarks and attachment points for nasal structures.
Specifically, the piriform aperture essentially frames the entrance to the nasal cavity. Consequently, its size and shape influence nasal appearance and airflow patterns.
The Cartilaginous Framework: Flexible Architecture
Cartilage forms the middle and lower portions of the external nose and creates much of the internal nasal structure.
The Upper Lateral Cartilages
These paired cartilages form the middle third of the nose, creating the cartilaginous bridge. Essentially, they’re continuations of the septal cartilage, extending laterally on each side.
The upper lateral cartilages attach to:
- The nasal bones superiorly (at the top)
- The septal cartilage medially (toward the midline)
- Additionally, the lower lateral cartilages inferiorly (at the bottom)
Importantly, these cartilages are crucial for maintaining the internal nasal valve—the narrowest part of the nasal airway. Therefore, if they’re weakened, collapsed, or inadequately supported, breathing problems result.
The Lower Lateral Cartilages (Alar Cartilages)
These paired, curved cartilages form the nasal tip and support the nostrils. Each consists of:
- Medial crura: The inner portions that run along the columella, meeting in the midline and providing tip support.
- Middle crura: The transitional portion between medial and lateral segments.
- Lateral crura: The outer portions that extend along the alar rims (nostril margins), providing nostril shape and support.
Consequently, the strength, size, shape, and positioning of these cartilages profoundly affect tip appearance and function. For example, strong, well-positioned alar cartilages create a refined, well-supported tip. In contrast, weak or malpositioned cartilages lead to a bulbous or drooping tip, and sometimes to breathing problems if nostril support is inadequate.
Rhinoplasty tip work involves reshaping, repositioning, or reinforcing these cartilages through various surgical techniques.
The Septal Cartilage
The septal cartilage is the largest single cartilage in the nose. Specifically, it forms the anterior (front) portion of the nasal septum—the wall dividing the right and left nasal passages.
This quadrilateral plate of cartilage provides crucial support to the entire nose. It attaches:
- Superiorly and posteriorly to bones (perpendicular plate of the ethmoid and vomer)
- Anteriorly and inferiorly to the maxillary crest (a ridge of bone at the base of the nose)
- Additionally, it connects to the upper lateral cartilages and the medial crura of the lower lateral cartilages
When the septum deviates (bends to one side), it can obstruct airflow and create external asymmetry. Therefore, septoplasty surgery straightens deviated septa to improve breathing.
The septum is also surgically important because it’s a primary source of cartilage for grafting during rhinoplasty. Specifically, surgeons can harvest pieces of septal cartilage to use for tip grafts, dorsal augmentation, or structural support without creating external changes or visible donor sites.
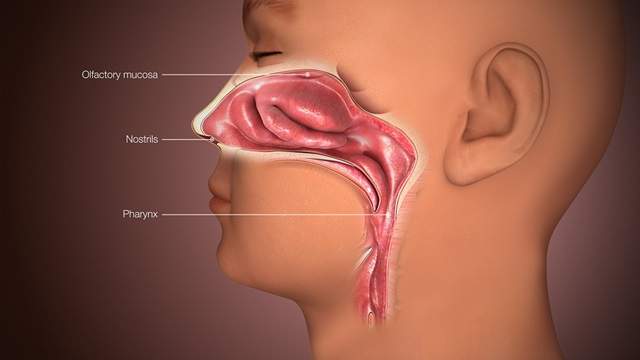
Anatomy of the Nose: The Nasal Cavity: Internal Anatomy
Open your mouth, breathe in, and feel where air enters through your nose. That passageway is the nasal cavity—much more complex than a simple tube.
Anatomy of the Nose: The Septum
The nasal septum divides the nasal cavity into right and left sides. Ideally, it sits in the midline, creating equal passages. In reality, most people have at least mild septal deviation—the septum leans more to one side.
The septum consists of:
- Anterior portion: Septal cartilage (discussed above)
- Superior/posterior portion: Perpendicular plate of the ethmoid bone (thin bone extending down from the skull base)
- Inferior/posterior portion: Vomer bone (thin bone running front to back)
Where these three components meet—cartilage, perpendicular plate, and vomer—is an area prone to deviation and fracture.
The Turbinates
The turbinates (or nasal conchae) are shelf-like structures projecting from the lateral (outer) walls of the nasal cavity. Most people have three: inferior (lower), middle, and superior (upper) turbinates.
The inferior turbinates are the largest and most clinically important. Specifically, they’re bony projections covered by erectile tissue—tissue that can swell and shrink based on blood flow, similar to how other erectile tissues in the body function.
Turbinate functions include:
- Directing airflow through the nasal passages
- Humidifying inspired air
- Warming air before it reaches the lungs
- Additionally, filtering particles through the mucus they produce
When turbinates become chronically enlarged (from allergies, chronic inflammation, or anatomical factors), they can obstruct airflow, causing nasal congestion. Therefore, turbinate reduction procedures can help restore breathing.
The Nasal Valve
The nasal valve is the narrowest part of the nasal airway—the bottleneck that provides most resistance to airflow. There are two:
- Internal nasal valve: The angle between the septum and the upper lateral cartilage (normally about 10–15 degrees). Consequently, narrowing this angle causes breathing problems.
- External nasal valve: The area at the nostril opening, supported by the alar cartilages and surrounded by nasal ala tissue.
Importantly, valve collapse or narrowing is a common cause of breathing difficulties, and addressing it often requires structural rhinoplasty techniques like spreader grafts (for internal valve) or alar batten grafts (for external valve).
The Paranasal Sinuses
The nose connects to four pairs of air-filled spaces within the facial bones:
- Maxillary sinuses: Large sinuses within the cheek bones, draining into the middle meatus of the nasal cavity
- Ethmoid sinuses: Multiple air cells between the eyes, draining into the middle and superior meatus
- Frontal sinuses: Sinuses in the forehead above the eyes, draining into the middle meatus
- Sphenoid sinuses: Deep sinuses behind the ethmoid sinuses, draining into the superior part of the nasal cavity
These sinuses lighten the skull, contribute to voice resonance, and produce mucus. When their drainage pathways become blocked, sinusitis (sinus infection) develops. Therefore, sinus anatomy is relevant to rhinoplasty because nasal surgery can affect drainage pathways.
Blood Supply: The Vascular Networks
The nose has abundant blood supply from multiple sources, which is why it heals well but also why nosebleeds can be profusely.
Arterial Supply
Blood reaches the nose through branches of both the internal and external carotid arteries:
From the external carotid:
- Facial artery branches (lateral nasal artery, superior labial artery)
- Sphenopalatine artery (the main blood supply to the nasal cavity, entering posteriorly through the sphenopalatine foramen)
From the internal carotid:
- Anterior and posterior ethmoidal arteries (supplying upper portions of the nasal cavity)
These vessels anastomose (connect) extensively, creating redundant blood supply. As a result, this is why noses survive trauma and surgery well—even if one vessel is damaged, others compensate.
Anatomy of the Nose: Kiesselbach’s Plexus (Little’s Area)
On the anterior septum, multiple blood vessels converge in an area called Kiesselbach’s plexus. Specifically, this is the most common site of nosebleeds (epistaxis), particularly in children.
The superficial location and rich vascular network make this area prone to bleeding from trauma, dry air, or nose-picking.
Venous Drainage
Venous blood drains through corresponding veins that accompany the arteries. Some drainage goes into the facial veins externally, while internal drainage goes into the sphenoid sinus and cavernous sinus.
This connection to intracranial venous structures means that severe nasal infections can theoretically spread to the brain—rare, but a reason to take nasal infections seriously.
Nerve Supply: Sensation and Smell
The nose receives both sensory innervation (for feeling) and specialized olfactory innervation (for smelling).
Sensory Innervation
General sensation comes from branches of the trigeminal nerve (cranial nerve V):
- The ophthalmic division (V1) supplies the upper nose through ethmoidal and infratrochlear nerves
- The maxillary division (V2) supplies the lower nose through branches of the infraorbital nerve and nasopalatine nerve
This innervation provides sensation of touch, temperature, and pain.
Olfactory System
Smell perception happens in the olfactory region—the upper portion of the nasal cavity containing specialized olfactory epithelium. Specifically, this mucosa contains olfactory receptor neurons whose axons form the olfactory nerve (cranial nerve I), projecting through the cribriform plate into the olfactory bulb of the brain.
Consequently, damage to this region—from trauma, surgery, or chronic inflammation—can cause anosmia (loss of smell).
The Nose in Function: Why Anatomy Matters
Understanding nasal anatomy isn’t just academic—it explains how the nose performs its multiple functions.
Anatomy of the Nose: Breathing and Airflow
The nasal passages condition inspired air. Specifically, turbulence created by turbinates and septum slows airflow, allowing time for warming, humidification, and filtration. Moreover, the narrow nasal valve creates most airflow resistance—this is why nose breathing takes more effort than mouth breathing.
Anatomy of the Nose: Filtration and Protection
Nasal hairs (vibrissae) at the nostrils trap large particles. Additionally, mucus produced by goblet cells in the nasal mucosa traps smaller particles and pathogens. Furthermore, cilia (microscopic hair-like structures) beat in coordinated waves to move mucus posteriorly toward the throat, where it’s swallowed (along with trapped debris).
This mucociliary clearance protects lungs from inhaled particles and organisms.
Humidification and Warming
The large surface area of turbinates and the rich blood supply warm inspired air to body temperature and humidify it to nearly 100% humidity by the time it reaches the nasopharynx. Therefore, this protects delicate lung tissue from cold, dry air.
Anatomy of the Nose: Olfaction
Airflow to the olfactory region allows smell perception, which contributes not just to smell itself but also to taste (most of what we call “taste” is actually smell).
Anatomy of the Nose: Voice Resonance
The nasal cavity and sinuses contribute to voice quality through resonance. This is why you sound different when congested—the altered resonance changes voice characteristics.
Clinical Relevance: When Anatomy Becomes Important
Nasal anatomy becomes particularly relevant in several clinical situations:
- Rhinoplasty planning: Surgeons need to understand individual anatomical variations to plan appropriate techniques. For example, thick skin requires different approaches than thin skin. Similarly, strong cartilage behaves differently than weak cartilage.
- Breathing problems: Understanding valve anatomy, turbinate function, and septal position helps diagnose the cause of nasal obstruction.
- Trauma management: Knowing blood supply helps manage nosebleeds. Additionally, understanding bone and cartilage architecture guides fracture treatment.
- Sinus disease: Comprehending sinus anatomy and drainage pathways helps diagnose and treat chronic sinusitis.
- Functional issues: Problems like anosmia, chronic drainage, or recurrent infections often trace to anatomical factors.
Anatomy of the Nose – Individual Variation: No Two Noses Alike
While the basic anatomical components are universal, their specific configuration varies enormously between individuals.
Bone size and shape differ. Cartilage strength, size, and symmetry vary. Skin thickness ranges from thin to very thick. Septum deviation is common. Turbinate size varies. Blood vessel patterns differ.
These variations explain why noses look so different from person to person and why surgical techniques need individualization. Specifically, what works beautifully for one patient’s anatomy might not work for another’s.
Ethnic background influences nasal anatomy significantly. Different ethnic groups have characteristic patterns of bone structure, cartilage configuration, and soft tissue thickness. Therefore, modern rhinoplasty respects these variations, aiming to enhance appearance while maintaining ethnic identity rather than imposing a universal “ideal” nasal shape.
The Bottom Line on Nasal Anatomy
The anatomy of the nose is far more intricate than its simple external appearance suggests. Multiple bones, several cartilages, elaborate vascular networks, sophisticated neural innervation, and connections to sinus systems all work together to create both the structure you see and the functions you depend on.
For anyone considering rhinoplasty, understanding this anatomy helps clarify what’s actually possible, why certain techniques get chosen, and what realistic expectations look like. For those dealing with breathing problems, it explains where things can go wrong and how interventions might help. And for the simply curious, it offers a window into the remarkable complexity hidden beneath a deceptively simple exterior.
Your nose is an engineering marvel—elegantly designed to perform multiple crucial functions while projecting from the center of your face in a way that significantly influences facial aesthetics. Therefore, understanding its anatomy is the first step toward appreciating both its form and its function.