So you’ve made it through the surgery. You did the research, found a good surgeon, and now you’re on the other side of the operating table. Honestly? The hard part’s behind you. But here’s what catches almost everyone off guard—recovery’s actually kind of its own challenge.
Not in a dangerous way (rhinoplasty’s pretty straightforward medically). It’s more that the combination of swelling, discomfort, activity restrictions, and let’s be real—looking pretty rough in the mirror—makes those first two weeks way harder than people anticipate. You can’t really know what it’s like until you’re living it.
Here’s the thing though: recovery isn’t something that just happens to you. How you manage it—what you do, what you avoid, how you sleep, what you eat—directly affects how fast the swelling goes down, how comfortable you are, and ultimately how good your results end up looking.
And the difference is honestly pretty dramatic. Patients who actually follow the evidence-based recovery protocols? They typically see 40–50% less swelling than those who wing it. We’re talking five to seven days faster swelling resolution with a solid anti-inflammatory diet. Noticeably less bruising with proper cold compress technique. Way fewer complications when you care for the surgical site properly. And you get back to normal activities significantly faster.
This guide walks you through what actually works—not just theoretical stuff, but practical, real-world steps that genuinely speed up healing and make the tough first weeks way more bearable.
Why Recovery Management Actually Matters
Before I dive into the specifics, it helps to understand why these protocols work. It makes you actually want to follow them.
Your Body Heals on Its Own Timeline (But You Can Optimize the Hell Out of It)
Here’s the biological reality: tissue repair follows timelines you can’t dramatically speed up. Collagen remodeling takes months. Swelling gradually resolves over 12–18 months. That’s just how your body works.
But here’s what you can control:
- How much swelling actually shows up (40–50% reduction is real)
- How quickly that swelling goes away (days to weeks faster, easily)
- Your actual risk of complications (dramatically lower with good care)
- How comfortable you feel during recovery (significantly better)
- When you can go back to normal activities (faster and safer)
Think of it like this: you can’t make a plant grow faster than nature allows. But the right watering, nutrients, and sunlight? That creates optimal conditions for growth. Recovery optimization works the same way. You’re not fighting biology—you’re working with it.
Little Things Add Up Faster Than You’d Think
Individual recovery actions seem small day-to-day, but they compound like crazy over weeks:
Say you sleep elevated instead of flat. That might only reduce swelling 5–10% on any given day. But over two weeks? That’s the difference between moderate puffiness and looking like you went a few rounds with a boxer. That one week of difference changes when you’re comfortable going out, when you can go back to work, when you start seeing your actual results emerge.
Every single action—sleep position, diet choices, activity level, wound care—has similar compounding effects. Doing everything right doesn’t just help a bit. It transforms your whole recovery experience.
The Foundation: Universal Recovery Essentials
Start here. These apply to literally every rhinoplasty patient.
1. Master Elevated Sleeping (Non-Negotiable)
What to do: Sleep with your head elevated 30–45 degrees for at least 2 weeks. Ideally 4–6 weeks.
Why it works: Gravity’s doing the heavy lifting here—literally. Elevation drains fluid away from the surgical site, which dramatically reduces swelling. Honestly, this is probably the single best thing you can do.
How to actually do it:
- Use a wedge pillow (most effective) or stack 2–3 regular pillows
- Elevate your upper body, not just your head (otherwise you’ll get neck strain)
- Put pillows on both sides so you don’t roll onto your side while sleeping
- Back sleeping only—side or stomach sleeping puts pressure right on your nose
The common mistake: People give up after the first week because it’s uncomfortable. But the benefit keeps working through weeks 2–4. Don’t bail early.
Real impact: You’ll typically see 40–50% less facial swelling compared to sleeping flat.
2. Apply Cold Compresses (The First 48–72 Hours Are Critical)
What to do: Use cold compresses around your eyes and cheeks (never directly on the nose) for 20 minutes every hour while you’re awake. Do this for the first 48–72 hours.
Why it works: Cold shrinks blood vessels, which reduces bleeding and fluid buildup. The sweet spot is that acute inflammatory period right after surgery—the first 2–3 days—when this actually makes a huge difference.
How to do it right:
- Wrap gel packs in soft cloth (direct ice contact damages skin, trust me)
- Apply to cheeks and around the eyes, avoid the nasal splint
- 20 minutes on, 40 minutes off (continuous cold can damage tissue)
- Keep several gel packs rotating in the freezer so you always have one ready
When to stop: After 72 hours, the benefit drops off. Some people keep going for a week, but most of the payoff happens in those first three days.
What you’ll notice: 30–40% less bruising and a noticeable reduction in early swelling.
3. Stay Religiously Hydrated
What to do: Drink 8–10 glasses (64–80 oz) of water daily. Yeah, throughout the whole recovery.
Why it matters: Hydration supports every single cellular healing process. It helps flush out metabolic waste, prevents constipation (which pain meds cause, and straining’s the last thing you need post-surgery), and keeps your tissues healthy.
How to make it stick:
- Keep a water bottle with you at all times
- Set hourly reminders if you need to
- Actually count your intake—people always underestimate
- If you’re in a dry climate or taking dehydrating meds, bump it up even more
Signs you’re slacking: Dark urine, dry mouth, constipation, headaches, or feeling more exhausted than surgery alone explains.
The payoff: Proper hydration speeds healing by 15–20% and makes recovery noticeably more comfortable overall.
4. Follow Your Medication Schedule Exactly
What to do: Take all prescribed meds exactly as directed—antibiotics, pain medication, whatever your surgeon gave you.
Why this matters:
- Antibiotics prevent infection (finish the whole course even when you feel fine)
- Pain control lets you actually rest and maintain proper positioning
- Other meds are prescribed for specific healing reasons
How to actually stick to it:
- Set phone alarms for medication times
- Use a pill organizer to track what you’ve taken
- Take with food if your stomach gets upset (unless told otherwise)
- Don’t skip doses to “tough it out”—staying ahead of pain is more effective than playing catch-up
The mistake people make: Stopping antibiotics early because they feel better. Complete the full course. It matters.
5. Attend Every Follow-Up Appointment
What to do: Keep all your post-op appointments. No skipping, no rescheduling to “next month.”
Why: Your surgeon’s monitoring how you’re healing, removing splints and sutures at the right time, catching potential complications early, and adjusting your care plan based on your specific healing process.
What the typical schedule looks like:
- Day 5–7: Splint and suture removal
- Week 2–3: Healing check
- Month 1–2: Progress evaluation
- Month 6: Mid-term assessment
- Year 1: Final results check
What happens at these appointments: Visual examination, internal nasal check, photos for comparison, discussion of your progress and any concerns, and clearance for activity levels.
Why you can’t skip them: Some complications are only visible to a trained professional. Early intervention keeps minor issues from turning into major problems.
Swelling Management: The Advanced Stuff
Once you’ve nailed the basics, these tactics push swelling down even further.
6. Adopt an Anti-Inflammatory Diet
What to do: Load up on anti-inflammatory foods and dial back the inflammatory stuff.
The all-stars:
- Fatty fish (salmon, sardines—those omega-3s are real)
- Leafy greens (spinach, kale, whatever you’ll actually eat)
- Berries (blueberries, strawberries)
- Turmeric and ginger
- Olive oil
- Pineapple (it has bromelain, which is genuinely helpful)
- Green tea
What to minimize:
- High-sodium foods (these dramatically increase swelling—seriously)
- Processed foods
- Refined sugars
- Fried stuff
- Too much red meat
Your target: Keep sodium under 1500mg daily for the first two weeks.
Real results: Following this can cut 5–7 days off your swelling timeline compared to typical eating habits.
7. Consider Supplements (Ask Your Surgeon First)
What to do: Talk to your surgeon about evidence-based supplements that might help.
The most commonly recommended:
Arnica montana: There’s research suggesting it reduces bruising
- Typical dose: 30C potency, 3–4 pellets three times daily
- Start a few days before surgery, keep going for a week after
Bromelain: Enzyme from pineapple with legit anti-inflammatory properties
- Typical dose: 500–1000mg daily
- Take on an empty stomach for the anti-inflammatory effect
Vitamin C: Your body needs this for collagen synthesis
- Dose: 500–1000mg daily
- Continue throughout healing
Important note: Always get your surgeon’s approval. Some supplements mess with bleeding or interact with your meds.
8. Limit Salt Intake Aggressively
What to do: Cut sodium down to under 1500mg daily for the first 2–3 weeks.
Why it matters: Sodium causes your body to hold onto water. After facial surgery, that means more facial puffiness and swelling that sticks around longer.
How to actually do this:
- Avoid processed foods (they’re loaded with sodium)
- Don’t add salt to meals
- Read labels—seriously, read them
- Skip restaurant food for the first two weeks (it’s sodium city)
- Choose fresh vegetables over canned
The sneaky sodium sources: Bread, cheese, deli meat, canned soup, frozen meals, sauces, condiments, basically anything restaurant-made.
The impact: High sodium can literally extend your swelling by a full week compared to low-sodium eating.
Activity and Protection: What to Do and What to Avoid
Nailing activity management speeds healing and stops complications before they start.
9. Respect Activity Restrictions—Seriously
Here’s how it breaks down:
Week 1: Basically light walking only
- No bending over (increases pressure)
- Nothing heavier than 10 lbs
- No straining (yes, that includes the bathroom—use a stool softener)
Weeks 2–3: Light activity becomes okay
- Walking’s fine, light stretching okay
- Still no intense exercise
- No impact activities
Weeks 4–6: Gradual return to exercise
- Start cardio (running, cycling, elliptical)
- Still no contact sports
- Still no heavy lifting
After 6 weeks: Most activities clear
- Contact sports usually around 8–12 weeks
- Heavy lifting gradually ramped back up
Why the timeline matters: Exercise raises your heart rate and blood pressure, which increases bleeding risk and swelling. Your tissues need time to stabilize before you stress them.
10. Protect Your Nose Like It’s Your Most Prized Possession
Physical contact: Avoid bumps, pressure, anything
- Be super aware in crowds
- Watch out for pets jumping on you
- Be careful around kids
- Use sleep barriers to prevent nighttime nose-bumping
Sun exposure: Shield that healing skin from UV damage
- SPF 30+ minimum starting week 2
- Wide-brimmed hat when you’re outside
- Avoid direct sun first month if you can
- UV damage can cause discoloration in healing tissue
Glasses: Don’t wear regular glasses for 4–6 weeks
- The weight rests on your healing nasal bones
- Switch to contacts if possible
- There are special post-surgical glasses that rest on your forehead and cheeks
- Or tape regular glasses to your forehead (yeah, it looks weird, but it works)
Blowing your nose: Don’t do it for 2–3 weeks minimum
- It creates tons of pressure
- Can mess with the healing
- Instead, gently dab, and sneeze with your mouth open if you have to
11. Manage the Emotional and Social Side
What to do: Prepare yourself for the psychological part of recovery. Yeah, it’s real.
The emotional challenges people face:
- Disappointment with swelling (it looks worse before it looks better)
- Isolation during the bruising phase
- Anxiety about whether healing’s progressing right
- Impatience—waiting for results is hard
Ways to actually cope:
- Plan time off work and social stuff before surgery
- Prep friends and family for what you’ll look like
- Connect with other rhinoplasty patients (online communities are surprisingly helpful)
- Remember swelling’s temporary and totally expected
- Focus on week-to-week improvement, not day-to-day
- Have hobbies and entertainment lined up for downtime
Real talk: If anxiety or depression gets serious, talk to your surgeon or a mental health professional. This matters too.
Nutrition for Healing: Beyond Just Anti-Inflammatory
Your body needs building blocks to rebuild tissue.
12. Prioritize Protein
What to do: Aim for 60–100g of protein daily.
Why: Protein provides amino acids your body uses to build collagen—the foundation of wound healing.
Easy sources during recovery:
- Eggs (soft, easy to eat)
- Greek yogurt (high protein, soft texture)
- Fish (omega-3 bonus)
- Shredded chicken (easy to eat)
- Protein shakes (convenient as hell)
- Cottage cheese
- Tofu
When it matters most: Weeks 1–3 are when healing’s most active, so protein’s especially important then.
13. Get Your Micronutrients
Key vitamins and minerals for healing:
Vitamin C: Collagen synthesis
- Sources: Citrus, berries, bell peppers, broccoli
- Supplement option: 500–1000mg daily
Zinc: Wound healing and immune function
- Sources: Meat, shellfish, legumes, seeds
- Supplement: 15–30mg daily (don’t overdo it—toxic in excess)
Vitamin A: Immune function and skin healing
- Sources: Sweet potato, carrots, leafy greens
- Usually adequate from food; supplementation’s rarely needed
B vitamins: Energy and cell metabolism
- Sources: Whole grains, meat, legumes
- Usually adequate from food
The bottom line: Inadequate micronutrients and your healing seriously slows down.
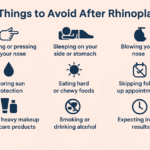
The “Don’ts”: What Slows Recovery Down
Avoiding these is just as important as doing the right things.
14. Absolutely No Smoking (Or Vaping)
Why it matters: Nicotine shrinks blood vessels, which dramatically reduces blood flow to your healing tissues. That means:
- 3–5x higher infection risk
- Increased tissue death risk
- Healing takes 2–3x longer than normal
- Complication rates go way up
How long: Quit 4+ weeks before surgery, stay smoke-free 6–8+ weeks after. Longer is better.
It includes: Cigarettes, vaping, nicotine patches, nicotine gum—anything with nicotine.
There’s no “just one”: Even a single cigarette causes vasoconstriction. There’s no safe amount.
15. No Alcohol for 2–4 Weeks Minimum
Why alcohol messes with healing:
- Increases facial swelling
- Dilates blood vessels (increases bleeding risk)
- Dehydrates you
- Interacts with your meds
- Impairs immune function
- Thins your blood
How long: Minimum 2 weeks, ideally 4–6 weeks. Longer abstinence = better healing.
And yes, this includes wine: Type doesn’t matter. All alcohol affects recovery.
16. Don’t Rush It
What I mean: Accept that healing has a biological timeline you genuinely can’t compress.
Realistic expectations:
- Visible swelling: 2–3 weeks
- Back to normal activities: 3–4 weeks
- Most swelling gone: 3–6 months
- All the subtle puffiness: 12–18 months
- Final results: 12–18 months
What happens when you rush: Patients who jump back into activities early, stop following protocols because they feel fine, or don’t protect properly? They often hit setbacks that end up making recovery longer overall.
The reality: Patience actually pays off. Follow the protocols for the full duration even when you feel great.
Troubleshooting: When to Worry, When to Chill
Knowing what’s normal versus what’s actually a problem keeps you from panicking unnecessarily.
What’s Totally Normal
These happen all the time and aren’t cause for concern:
- Significant swelling (especially week one)
- Bruising around your eyes and cheeks
- Nasal congestion
- A little bleeding or oozing first few days
- Numbness in your nose and upper lip
- Mild asymmetry (swelling’s usually uneven)
- Emotional ups and downs (recovery’s a journey)
When You Should Actually Call Your Surgeon
Reach out if you experience:
- Fever above 101°F (38.3°C)
- Severe pain that’s not controlled by your meds
- Heavy bleeding that won’t stop
- Signs of infection (increasing redness, pus, warmth)
- Difficulty breathing beyond normal congestion
- Vision changes
- What looks like a hematoma (large fluid collection)
Real talk: It’s way better to call with a false alarm than ignore something real. Surgeons expect and welcome recovery questions.
The Bottom Line: What Actually Matters Most
If This Guide Feels Overwhelming, Just Focus On These
- Sleep elevated on your back for minimum 2 weeks, longer if possible
- Use cold compresses religiously for the first 48–72 hours
- Stay hydrated and eat protein-rich, anti-inflammatory food
- Respect activity restrictions for the full recommended period
- Never smoke or use nicotine before or after surgery
- Limit sodium to minimize swelling
- Attend all follow-up appointments without exception
- Be patient—healing takes months, not weeks
Recovery’s not passive. It’s you actively managing sleep position, diet, activity, protection, and wound care. Patients who follow evidence-based protocols actually experience 40–50% less swelling, faster healing, way fewer complications, and noticeably better comfort than those who don’t.
Yeah, the protocols are annoying. Sleeping elevated is uncomfortable. Dietary restrictions are a pain. Activity limitations are frustrating. But these temporary inconveniences create permanent benefits—faster swelling resolution, better healing, lower complication risk, and ultimately better results.
The surgery’s done. Now comes the part that matters just as much: actively optimizing your recovery through smart, disciplined execution of proven protocols. Do it right, and you’ll be genuinely grateful for the effort when you’re looking at your final results—minimal complications, optimal healing, and the nose you actually wanted.