You’ve tried it all. The allergy medications. The nasal sprays you actually remember to use (okay, sometimes). Steam inhalation before bed. Even that phase where you propped yourself up on what felt like seven pillows just to sleep without gasping for air.
But here’s the thing—you still can’t breathe through your nose. Not really. One or both nostrils feel permanently blocked, like you’ve got a cold that never quite leaves. Ever. Your sleep is suffering because of it. You’re waking up with a dry mouth from breathing through it all night. Exercise? Forget about it. You can’t get enough air through your nose to keep up with what your body actually needs.
If that sounds uncomfortably familiar, the culprit might not be allergies, a deviated septum, or even chronic sinusitis. Could be turbinate hypertrophy—which is just a fancy way of saying your nasal turbinates have become enlarged and are basically blocking your airways. And here’s the good news: there’s actually a solution. Turbinate reduction surgery can reshape these structures and get your breathing back to normal.
The thing is, when an ENT surgeon mentions turbinate reduction, most people go blank. What exactly are turbinates? Why’s mine causing problems? What does the actual surgery involve? How long until I can breathe normally? Will this even work? The terminology feels foreign, the anatomy is hidden where you can’t see it, and honestly, nasal surgery sounds intimidating.
This guide walks you through everything—from basic anatomy and why turbinates cause problems through the different surgical techniques, what recovery actually looks like, the risks (and how real they are), and what you can expect long-term. If chronic nasal obstruction has been messing with your quality of life and regular treatments haven’t done much, understanding this procedure might be the answer you’ve been looking for.
What Are Turbinates? Understanding the Anatomy
Before diving into the surgery part, it helps to actually understand what turbinates are and why they matter. Seriously, once you get this, the rest makes way more sense.
The Structure of Turbinates
Inside your nose, you’ve got these shelf-like structures protruding from each side of your nasal passage. They’re called turbinates (doctors also call them nasal conchae—love when medical terms have multiple names, right?). They’re covered in specialized mucous membrane tissue and have a whole network of blood vessels running through them.
Here’s what you’re working with:
- Inferior turbinates: The largest ones, located lowest in your nose. These are the troublemakers when it comes to obstruction.
- Middle turbinates: Smaller. Located above the inferior turbinates.
- Superior turbinates: The smallest set. Way up there at the top of your nasal cavity.
The inferior turbinates are what usually causes breathing problems. They’re roughly the size of your index finger—so when they swell up, you can imagine what that does to your airways.
What Turbinates Actually Do (They’re Not Useless, I Promise)
People sometimes think turbinates are just random tissue taking up space. They’re not. These structures do important stuff:
- Warming air: Cold air gets warmed up before it reaches your lungs. Turbinates handle that.
- Adding moisture: They humidify dry air so your airways don’t dry out.
- Cleaning the air: The mucous membrane traps dust, allergens, and bacteria. Your body’s way of filtering.
- Directing airflow: They create specific airflow patterns that actually help your nasal passages work properly.
Why this matters for surgery: A good surgeon won’t just remove a bunch of turbinate tissue. That actually causes problems. The goal is reducing the size while keeping them functional. Remove too much, and you end up with something called “empty nose syndrome,” which is honestly worse than the original obstruction. So your surgeon has to find that sweet spot.
What Is Turbinate Hypertrophy? (Why Surgery Becomes Necessary)
Turbinate hypertrophy is basically when your turbinates become chronically enlarged and don’t shrink back down to normal size.
Why Your Turbinates Got Enlarged in the First Place
There are several reasons this happens:
- Chronic allergies: Your nose stays inflamed from allergies, and eventually that swelling becomes permanent.
- Vasomotor rhinitis: This is non-allergic irritation from stuff like smoke, strong perfumes, weather changes, spicy food. Your body overreacts to these triggers.
- Chronic sinusitis: When your sinuses are constantly inflamed, it affects your turbinates too.
- Nasal spray addiction: Sounds odd, but nasal sprays can actually make things worse if you use them too long. It’s called rhinitis medicamentosa, and it causes rebound swelling.
- One-sided compensation: If you have a deviated septum on one side, sometimes the turbinate on the opposite side enlarges to try to balance things out. Your body’s attempt to compensate.
- Just how you’re built: Some people have naturally larger turbinates. Genetics, anatomy, the luck of the draw.
- Hormonal shifts: Pregnancy, for instance, can cause turbinate swelling that sticks around.
Symptoms That Might Mean You Need Surgery
The main sign is chronic nasal obstruction that medical treatment doesn’t really fix. But there’s usually more:
- One or both nostrils feel blocked basically all the time
- Sleep is affected because breathing is hard
- You’re mouth breathing, especially at night (not fun)
- Snoring or sleep apnea that’s worse because of the nasal obstruction
- Your sense of smell isn’t what it used to be
- Physical activity is harder because you can’t get enough air
- Postnasal drip that won’t quit
- Sinus infections keep coming back
The real indicator: You’ve been dealing with this for at least 3-6 months, and you’ve already tried the standard medical treatments—allergy medications, nasal steroids, antihistamines—and they haven’t helped enough.
How Doctors Figure Out You Need Surgery
- Nasal endoscopy: Your doctor uses a small camera to look inside your nose and actually see how enlarged the turbinates are and how they’re blocking your airway.
- CT scan: Sometimes they order this to get the full picture of your nasal anatomy and make sure there’s nothing else going on.
- Allergy testing: If allergies might be contributing, doctors want to know so they can optimize medical management first.
- Trial period with medical therapy: Most surgeons won’t operate until you’ve genuinely tried conservative treatment. It matters.
- Direct observation: Your doctor can literally see the enlargement and watch how it affects your breathing through the endoscope.
Types of Turbinate Reduction: Different Surgical Approaches
There isn’t just one way to do this surgery. Different techniques exist, each with different mechanisms, recovery timelines, and outcomes. Here’s what surgeons are working with:
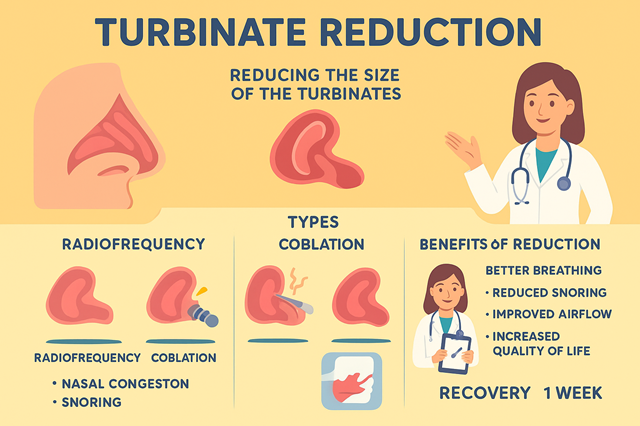
1. Radiofrequency Ablation (RFA) or Coblation
An energy probe gets inserted into the turbinate tissue. It creates controlled heat damage, which causes the tissue to shrink over the next few weeks as scar tissue forms.
Why surgeons like it:
- Not very invasive at all
- Can actually be done in the office under local anesthesia
- Doesn’t cause much bleeding
- Keeps the turbinate structure and outer membrane intact
- The procedure itself is quick—maybe 15-20 minutes
The downsides:
- Results might not be as dramatic as other methods
- You might need a second treatment down the line
- Takes weeks before you see the full effect (not immediate)
Best suited for: Mild to moderate enlargement if you want the least invasive approach.
2. Laser Turbinate Reduction
Laser energy ablates (removes) turbinate tissue. As it heals, the turbinate shrinks.
The benefits:
- Very precise tissue removal
- Minimal bleeding
- Can be done under local anesthesia
- Relatively quick recovery compared to some options
Potential issues:
- Results can be unpredictable
- Excessive scarring is possible
- Might need multiple sessions
- More expensive than some alternatives
Good for: Moderate enlargement when you need precise reduction.
3. Microdebrider Submucous Resection
This technique uses a small rotating blade to remove turbinate bone and soft tissue while keeping the outer mucous membrane intact.
Advantages:
- Preserves the mucous membrane, which is important
- Gives predictable, significant reduction
- Lower risk of crusting and dryness compared to complete removal
- Usually just one procedure needed
Disadvantages:
- Needs an operating room and general anesthesia, typically
- More invasive than ablation techniques
- More bleeding risk initially
- Recovery takes longer (2-3 weeks usually)
Best for: Moderate to severe enlargement when you need substantial improvement.
4. Partial Turbinectomy
Surgical removal of part of the turbinate tissue.
Pros:
- Immediately opens up your nasal passages—significant change right away
- Results are predictable and often dramatic
- You rarely need a second procedure
Cons:
- Most invasive option available
- Higher complication risk
- Real risk of removing too much tissue (which leads to that empty nose syndrome we mentioned)
- Longer recovery time
- More initial bleeding
Best for: Severe obstruction that hasn’t responded to other treatments. Usually a last resort.
Which Technique Actually Works Best?
Honestly? It depends. Severity matters. Your specific anatomy matters. Surgeon preference matters. Patient factors matter.
The trend in modern practice: Surgeons are moving toward tissue-preserving techniques (like RFA and microdebrider work) rather than aggressive removal. The logic is solid—you want relief without destroying function.
Your surgeon’s recommendation will be based on your specific anatomy and how severe the obstruction is. Don’t hesitate to ask about their experience with different techniques and their complication rates. That’s totally fair game.
The Turbinate Reduction Procedure: What to Expect
Understanding what’s actually going to happen helps take away some of the anxiety. I get it.
Pre-Operative Preparation
- Stop certain medications: Anything that increases bleeding (aspirin, NSAIDs, fish oil supplements, some others). Usually 1-2 weeks before.
- Get allergies under control: Surgery works better when inflammation is already managed going in.
- Arrange a ride: You can’t drive yourself home after anesthesia. Not happening.
- Block off recovery time: Plan on 3-7 days away from work, depending on which technique your surgeon uses.
During the Surgery
Anesthesia: Depends on the technique and whether you’re having other procedures done. Might be local anesthesia with sedation, or full general anesthesia.
How long: Anywhere from 30 minutes to 2 hours. More if you’re also having septoplasty or other procedures done at the same time.
What happens in there:
- Surgeon accesses your turbinates through your nostrils (no external cuts, which is nice)
- Performs the reduction technique on your inferior turbinates (sometimes middle turbinates too)
- Might place nasal packing depending on technique and preference
- You head to recovery
Pain during surgery: None. You’re completely anesthetized.
Immediately After Surgery
- First few hours: You’ll feel groggy from anesthesia. Counterintuitively, your nose will feel congested despite the reduction (that’s swelling, not obstruction). Maybe some mild discomfort.
- Evening: Congestion, some minor bleeding or oozing, dry mouth from mouth breathing, mild discomfort that’s usually manageable with prescribed pain medication.
- First night: Sleep propped up. Use a humidifier. Your nose still won’t feel open yet. Don’t be alarmed—this is completely normal.
Recovery Timeline: What Healing Actually Looks Like
Recovery varies depending on which technique was used, but there are definitely patterns.
Days 1-3: The Initial Recovery Phase
What’s happening:
- Significant nasal congestion (swelling, not obstruction—important distinction)
- Crusting and dried blood
- Minor bleeding or blood-tinged drainage
- Mild to moderate discomfort (rarely severe pain)
- You’ll be mouth breathing still
What to do: Take your pain medication as prescribed, use saline spray frequently, sleep with your head elevated, don’t blow your nose, skip strenuous activity, run that humidifier.
Reality check: You can’t breathe yet. This isn’t failure. It’s normal healing. The swelling is obscuring your improvement.
Days 4-7: Early Improvements Start
What you’ll notice: Swelling going down, first signs of better breathing (comes and goes), less crusting, less discomfort.
Many people return to work: By day 5-7, depending on what your job entails.
Weeks 2-3: Things Keep Improving
What’s happening: Your breathing keeps getting better progressively, crusting and drainage decreasing, still some swelling but way better than before.
By week 3: You should definitely notice clear improvement compared to how things were before surgery.
Weeks 4-6: Nearly There
What you’ll experience: Most swelling is gone, breathing is significantly better, your nasal passages feel more open, sleep quality improving.
By 6 weeks: You’re basically experiencing your final results.
Months 3-6: Complete Healing
Any remaining swelling is gone. Your turbinates have stabilized at their new size. Tissue remodeling is done. Now you can really evaluate how much your breathing improved.
Risks and Complications: The Real Talk
Like any surgery, there are risks. But—and this is important—serious complications are actually pretty rare.
Common Minor Issues (Happen in About 10-20% of Patients)
- Temporary crusting: Healing creates debris. You’ll need to irrigate.
- Minor bleeding: Some blood-tinged drainage in the first week or two is normal.
- Temporary worsening of congestion: The swelling makes things feel worse before they feel better.
- Smell changes: Usually temporary. Improves as swelling decreases.
- Mild discomfort: Manageable with over-the-counter pain medication.
Uncommon But More Serious (1-5% of Patients)
- Significant bleeding: Rare, but might need medical attention.
- Infection: Possible, though not common. Treated with antibiotics.
- Septal perforation: A hole in your nasal septum. Rare when it’s just turbinate surgery.
- Adhesions (synechiae): Scar tissue connects your septum to the turbinate. Might need to be separated.
- Surgery didn’t help: Breathing isn’t improved adequately. Could mean other factors are at play.
Rare But Serious Complications (Less Than 1%)
- Empty nose syndrome: This is the big one everyone worries about. Over-resection causes a paradoxical problem—your airways are open but breathing feels difficult. It’s essentially irreversible and honestly devastating. This is why your surgeon choosing to be conservative matters.
- CSF leak: Extremely rare. Happens if surgery goes too high and punctures something at the skull base.
- Vision problems: Super rare. Could result from bleeding or infection spreading.
- Anesthesia complications: Standard risks that come with any surgery requiring anesthesia.
How to Minimize Your Risk
- Get an experienced surgeon: Choose an ENT or facial plastic surgeon with significant turbinate reduction experience under their belt.
- Avoid over-aggressive techniques: Conservative reduction that preserves function beats aggressive removal every time.
- Actually follow post-op instructions: This reduces infection risk and helps everything heal properly.
- Show up for follow-ups: Catches any problems early.
Expected Outcomes: Will This Actually Work?
The question everyone really wants answered: does turbinate reduction actually improve breathing?
Success Rates
Breathing Improvement
70-90%
of patients report significant improvement
Objective Airflow
80-85%
show measurable increases on testing
Long-term Durability
Most
keep improvement for years
Need for revision: About 10-20% might need a second procedure eventually (happens more with conservative techniques like RFA).
What Affects Your Outcomes
Things that lead to better results:
- Turbinate hypertrophy is your main problem (vs. multiple factors causing obstruction)
- Realistic expectations
- Actually following post-operative care
- Not smoking
- Allergies under control
Things that lead to disappointing results:
- Severe septal deviation (might need septoplasty too)
- Unrealistic expectations
- Still using nasal sprays too much
- Allergies not well-controlled
- Smoking
What People Actually Say After Surgery
Positive:
- “I can finally breathe through my nose”
- “My sleep is so much better”
- “I stopped snoring”
- “I can exercise without feeling suffocated”
Mixed:
- “Breathing’s better but not perfect” (usually means other factors are involved too)
- “It took months to see the real improvement”
- “One side got better than the other”
Negative:
- “Didn’t change anything” (often indicates other obstruction causes)
- “Helped at first but came back” (might need revision or better allergy management)
Who Should Actually Consider This Surgery?
Not everyone with nasal congestion needs an operation.
The Ideal Candidate
- Chronic nasal obstruction for at least 6 months
- Tried conservative treatment (allergy meds, nasal steroids) genuinely, and it hasn’t helped enough
- Doctor confirmed turbinate hypertrophy through examination
- Either no significant septal deviation or willing to have septoplasty at the same time
- Realistic expectations about what surgery can do
- Healthy enough for surgery
Probably Not a Good Candidate
- Your obstruction comes mainly from other causes (deviated septum, nasal valve collapse)
- You’re expecting perfect breathing when your anatomy is complex
- Your allergies aren’t controlled (medical management should come first)
- You’ve currently got an active nasal or sinus infection
- Certain bleeding disorders
- You smoke (should quit first, honestly)
When to Try Medicine First
Most surgeons will push for exhausting conservative options before surgery:
- Nasal steroid sprays (fluticasone, mometasone)
- Oral antihistamines
- Allergy immunotherapy if allergies are the main driver
- Nasal irrigation
- Environmental control measures
Surgery makes sense once medical management—given a real chance—doesn’t provide enough relief.
The Bottom Line
Turbinate reduction surgery addresses enlarged nasal turbinates that are blocking your airways despite trying medical treatments. You’ve got options—from minimally invasive radiofrequency ablation to more aggressive approaches. The goal is improving your airflow while keeping those turbinate functions intact.
Most patients—70-90% of them—notice significant breathing improvement. Recovery usually takes 1-3 weeks before you’re back to normal, with final results showing by 3-6 months. Risks tend to be minor, but choosing an experienced surgeon who avoids over-resection matters. Seriously. That empty nose syndrome complication is rare but devastating.
If you’ve been struggling with chronic nasal obstruction that medications haven’t fixed, turbinate reduction might be the answer. Plenty of people have gotten this surgery and gone from struggling to breathe to actually enjoying easy, natural nasal breathing. Better sleep. Better exercise. Just better quality of life overall.
Talk with an experienced ENT surgeon who can look at your specific anatomy, confirm you actually have turbinate hypertrophy, and discuss whether reduction makes sense for you. For a lot of people, this relatively straightforward procedure changes everything—turning chronic frustration into easy breathing.