Olfactory Mucosa and Rhinoplasty: What Patients Should Know
Short answer: The olfactory mucosa—specialized tissue high in the nasal vault that detects odors—can be indirectly affected by rhinoplasty through changes in airflow, swelling, or rare trauma. With careful surgical planning that preserves internal nasal structures and stable postoperative care, most patients maintain or regain their baseline sense of smell within weeks to months.
Why smell comes up when people consider rhinoplasty
Here’s the thing: when you think about nose surgery, you probably picture bridge lines, tips, and symmetry. But the smell system—specifically the olfactory mucosa—sits higher in the nasal vault, quietly doing its job day in and day out. Patients ask whether olfactory mucosa and rhinoplasty can coexist without problems. In practice, they usually do. Still, a few details matter a lot: airflow, swelling, and surgical finesse.
In clinic, many people are surprised to learn that most postoperative smell changes come from reversible swelling or congestion, not from direct injury to olfactory tissue.
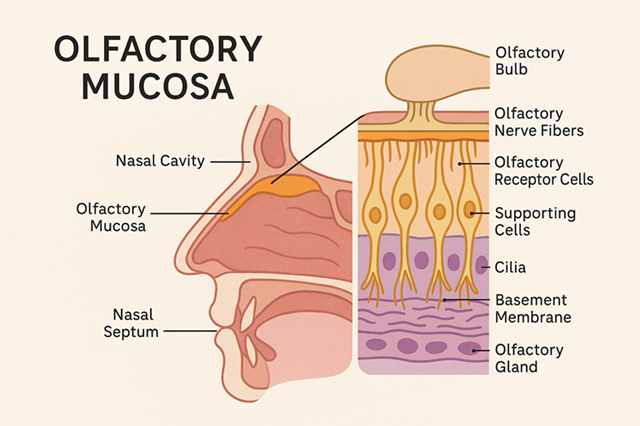
Olfactory mucosa 101: where it is and what it does
The olfactory mucosa is a specialized lining in the upper nasal cavity—near the cribriform plate and along the superior septum and superior turbinates. This is where odorant molecules interact with olfactory receptor neurons, converting smells into signals your brain can interpret. It’s not the same lining that humidifies or warms air lower in the nose; it’s more specialized and more delicate.
Olfactory Mucosa and Rhinoplasty: Key landmarks surgeons keep in mind
- Superior nasal vault: High in the nose, close to the skull base.
- Superior septum and turbinates: Areas with concentrated olfactory epithelium.
- Olfactory cleft: A narrow corridor where odor-carrying air needs access.
Maintaining a clear pathway to the olfactory cleft is essential. Even small changes in internal nasal geometry can change how odorant-laden air reaches those receptors, which is why techniques that stabilize the internal nasal valve and preserve mucosa matter.
How rhinoplasty can influence smell—directly and indirectly
Most modern rhinoplasty—whether open or closed—focuses on cartilage and bone reshaping while preserving mucosal integrity. That said, the relationship between olfactory mucosa and rhinoplasty is shaped by a few mechanisms.
Olfactory Mucosa and Rhinoplasty: Airflow redistribution
Subtle changes to the internal nasal valve or septum can redirect airflow. If less air reaches the olfactory cleft, perception can dip—usually temporarily while swelling resolves.
Edema and congestion
In the early weeks, swelling narrows corridors that odorants travel through. As edema fades, airflow normalizes and smell often rebounds.
Olfactory Mucosa and Rhinoplasty: Mucosal trauma (uncommon)
Direct injury to olfactory mucosa is rare with careful technique because the operative field is typically lower than the olfactory cleft.
Pre-existing inflammation
Allergic rhinitis, chronic sinusitis, or polyps can blunt smell before surgery. Managing these improves outcomes and expectations.
| Mechanism | How it affects smell | Typical course |
|---|---|---|
| Airflow changes | Less odorant reaches olfactory cleft | Improves as swelling subsides (weeks–months) |
| Edema/congestion | Temporary blockage of pathways | Common in first 2–6 weeks, then recovers |
| Mucosal injury | Rare, localized impact | Uncommon with preservation techniques |
| Underlying inflammation | Baseline smell reduced | Address medically for best results |
Protecting smell before, during, and after surgery
Before surgery: set the stage
- Share any history of allergies, chronic sinusitis, or polyps—these influence smell more than most people realize.
- Ask your surgeon about valve stabilization and septal preservation strategies if applicable.
- Discuss realistic timelines for postoperative smell recovery.
In the operating room: preservation mindset
- Favor techniques that preserve internal nasal valve angles and mucosal surfaces.
- Use atraumatic dissection and minimize cautery around delicate mucosa.
- Maintain or improve septal straightness to support laminar airflow.
After surgery: recovery that supports the olfactory cleft
- Stick to saline irrigations as instructed to reduce crusting that blocks odor flow.
- Avoid nose-blowing early on; follow your surgeon’s timeline.
- Manage allergies diligently; inflammation prolongs congestion.
- Be patient—weeks to months is a normal recovery window for smell.
What to expect: recovery timelines and real-world expectations
In many cases, smell dips slightly in the first 1–3 weeks, then improves as edema resolves. By 6–12 weeks, most patients are close to baseline. A small subset may take longer, especially if allergies or sinus disease flare.
Olfactory Mucosa and Rhinoplasty: When to check in
- Immediate concerns: Severe worsening after initial improvement, unilateral blockage, or persistent clear fluid—call your team.
- 6–8 weeks: If smell hasn’t budged, discuss topical steroid strategies or evaluation for inflammation.
- 3–6 months: Consider formal smell testing if symptoms persist.
Clinicians often note that structured nasal hygiene and allergy control are the quiet drivers of success here.
Common questions about olfactory mucosa and rhinoplasty
Will rhinoplasty permanently damage my sense of smell?
With preservation-focused techniques, permanent loss is uncommon. Most changes relate to congestion and resolve. Choose a surgeon who can explain how they protect mucosa and airflow.
Does open vs. closed rhinoplasty make a difference for smell?
Both can be done safely. Outcomes hinge more on surgical goals, anatomy, and attention to internal valve and septal support than on incision placement.
What if I already have a weak sense of smell?
Baseline hyposmia from allergies or sinus disease needs optimization. Treat what’s treatable first—your long-term result will be better.
Are there exercises to speed smell recovery?
Some patients try olfactory training (regular exposure to a set of distinct scents). Evidence is mixed but encouraging for post-viral cases; after rhinoplasty, it may help once your surgeon clears you and congestion improves.













Post Comment